- Clinical Study
- Insulin Secretion and Insulin Resistance Trajectories over 1 Year after Kidney Transplantation: A Multicenter Prospective Cohort Study
-
Jun Bae Bang, Chang-Kwon Oh, Yu Seun Kim, Sung Hoon Kim, Hee Chul Yu, Chan-Duck Kim, Man Ki Ju, Byung Jun So, Sang Ho Lee, Sang Youb Han, Cheol Woong Jung, Joong Kyung Kim, Su Hyung Lee, Ja Young Jeon
-
Endocrinol Metab. 2020;35(4):820-829. Published online November 18, 2020
-
DOI: https://doi.org/10.3803/EnM.2020.743
-
-
4,914
View
-
119
Download
-
5
Web of Science
-
6
Crossref
-
 Abstract Abstract
 PDF PDF Supplementary Material Supplementary Material PubReader PubReader  ePub ePub
- Background
We investigated the changing patterns of insulin secretion and resistance and risk factors contributing to the development of post-transplant diabetes mellitus (PTDM) in kidney recipients under tacrolimus-based immunosuppression regimen during 1 year after transplantation.
Methods
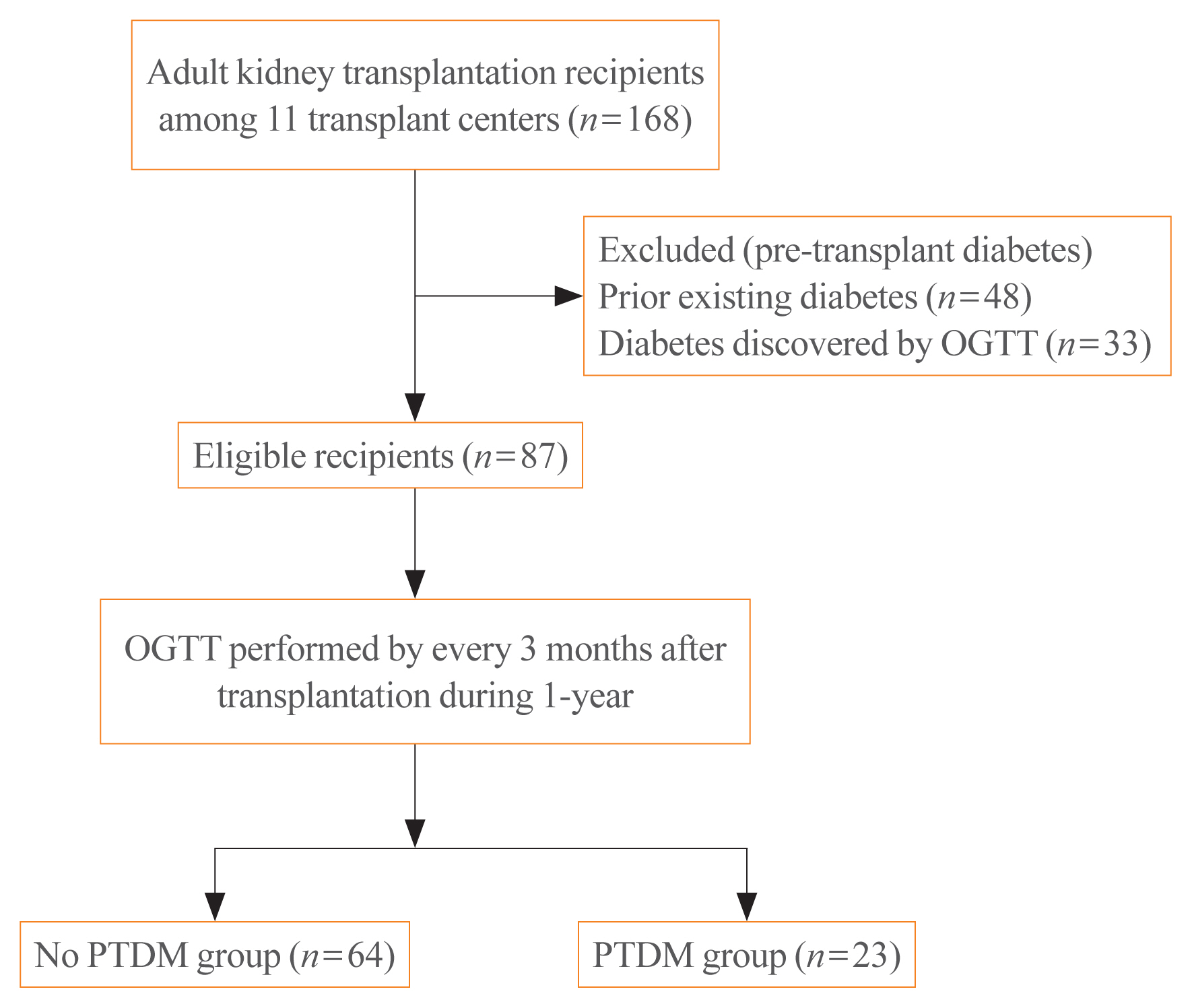
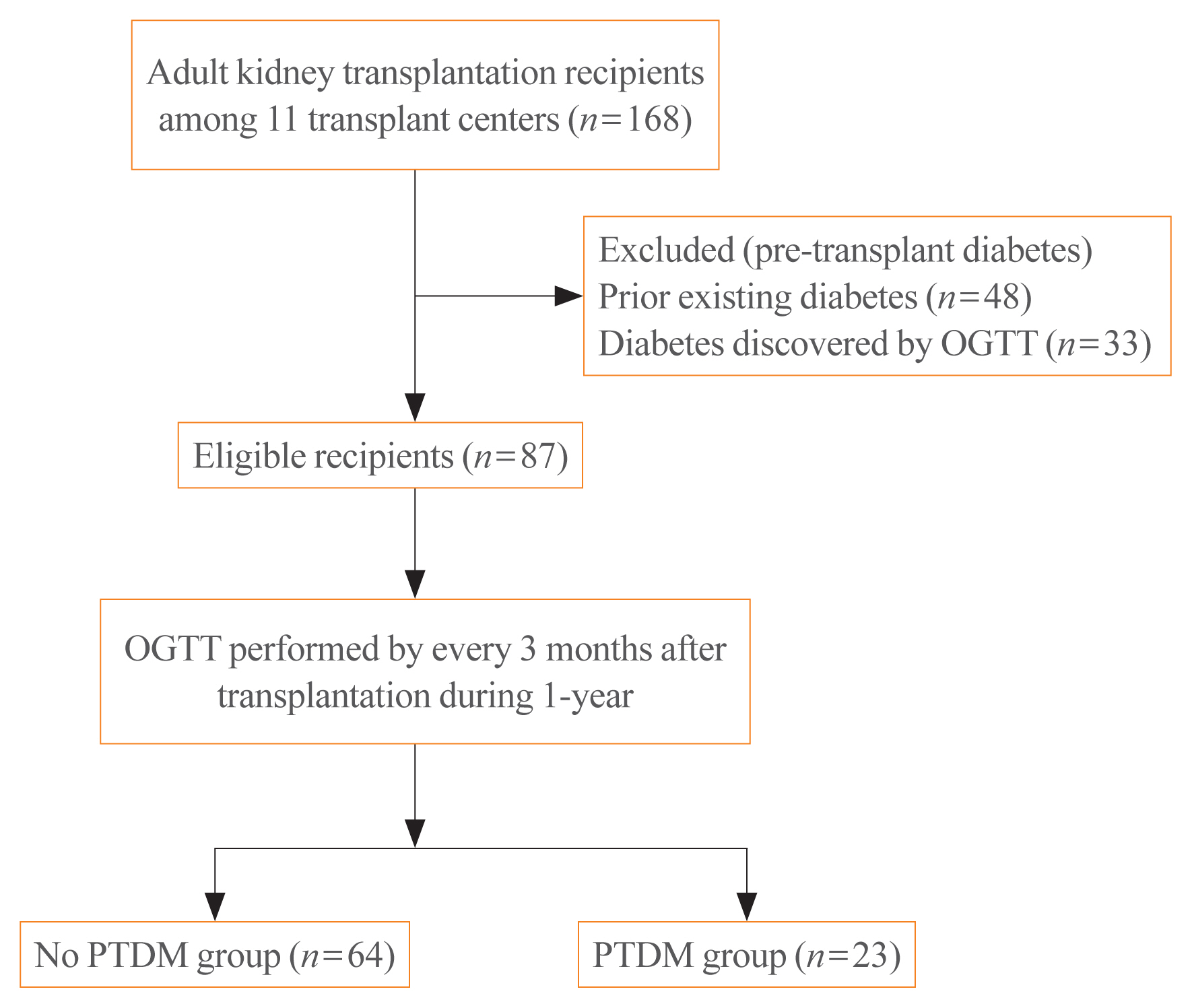
This was a multicenter prospective cohort study. Of the 168 subjects enrolled in this study, we analyzed a total 87 kidney transplant recipients without diabetes which was assessed by oral glucose tolerance test before transplantation. We evaluated the incidence of PTDM and followed up the index of insulin secretion (insulinogenic index [IGI]) and resistance (homeostatic model assessment for insulin resistance [HOMA-IR]) at 3, 6, 9 months, and 1 year after transplantation by oral glucose tolerance test and diabetes treatment. We also assessed the risk factors for incident PTDM.
Results
PTDM developed in 23 of 87 subjects (26.4%) during 1 year after transplantation. More than half of total PTDM (56.5%) occurred in the first 3 months after transplantation. During 1 year after transplantation, insulin resistance (HOMA-IR) was increased in both PTDM and no PTDM group. In no PTDM group, the increase in insulin secretory function to overcome insulin resistance was also observed. However, PTDM group showed no increase in insulin secretion function (IGI). Old age, status of prediabetes and episode of acute rejection were significantly associated with the development of PTDM.
Conclusion
In tacrolimus-based immunosuppressive drugs regimen, impaired insulin secretory function for reduced insulin sensitivity contributed to the development of PTDM than insulin resistance during 1 year after transplantation.
-
Citations
Citations to this article as recorded by  - Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis
Qiufeng Du, Tao Li, Xiaodong Yi, Shuang Song, Jing Kang, Yunlan Jiang
Acta Diabetologica.2024;[Epub] CrossRef - Distúrbio do eixo hipotálamo-hipófise-gonadal e sua associação com resistência à insulina em receptores de transplante renal
Lourdes Balcázar-Hernández, Victoria Mendoza-Zubieta, Baldomero González-Virla, Brenda González-García, Mariana Osorio-Olvera, Jesús Ubaldo Peñaloza-Juarez, Irene Irisson-Mora, Martha Cruz-López, Raúl Rodríguez-Gómez, Ramón Espinoza-Pérez, Guadalupe Varga
Brazilian Journal of Nephrology.2023; 45(1): 77. CrossRef - Hypothalamic-pituitary-gonadal axis disturbance and its association with insulin resistance in kidney transplant recipients
Lourdes Balcázar-Hernández, Victoria Mendoza-Zubieta, Baldomero González-Virla, Brenda González-García, Mariana Osorio-Olvera, Jesús Ubaldo Peñaloza-Juarez, Irene Irisson-Mora, Martha Cruz-López, Raúl Rodríguez-Gómez, Ramón Espinoza-Pérez, Guadalupe Varga
Brazilian Journal of Nephrology.2023; 45(1): 77. CrossRef - Postoperative fasting plasma glucose and family history diabetes mellitus can predict post-transplantation diabetes mellitus in kidney transplant recipients
Le Wang, Jin Huang, Yajuan Li, Kewei Shi, Sai Gao, Wangcheng Zhao, Shanshan Zhang, Chenguang Ding, Wei Gao
Endocrine.2023; 81(1): 58. CrossRef - Changes in glucose metabolism among recipients with diabetes 1 year after kidney transplant: a multicenter 1-year prospective study
Jun Bae Bang, Chang-Kwon Oh, Yu Seun Kim, Sung Hoon Kim, Hee Chul Yu, Chan-Duck Kim, Man Ki Ju, Byung Jun So, Sang Ho Lee, Sang Youb Han, Cheol Woong Jung, Joong Kyung Kim, Hyung Joon Ahn, Su Hyung Lee, Ja Young Jeon
Frontiers in Endocrinology.2023;[Epub] CrossRef - Pretransplant evaluation and the risk of glucose metabolic alterations after renal transplantation: a prospective study
Arminda Fariña-Hernández, Domingo Marrero-Miranda, Estefania Perez-Carreño, Antonia De Vera-Gonzalez, Alejandra González, Cristian Acosta-Sorensen, Ana Elena Rodríguez-Rodríguez, Tatiana Collantes, Marta del Pino García, Ana Isabel Rodríguez-Muñoz, Carla
Nephrology Dialysis Transplantation.2022;[Epub] CrossRef
- A Family Presenting with Catastrophic Features due to Pheochromocytoma Associated with Multiple Endocrine Neoplasia 2A.
-
Yun Jung Lee, Suk Chon, Sang Ho Lee, Tae Won Lee, Chun Gyoo Ihm, Tae June Noh, Seungjoon Oh, Jeong Taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim
-
Endocrinol Metab. 2010;25(2):135-141. Published online June 1, 2010
-
DOI: https://doi.org/10.3803/EnM.2010.25.2.135
-
-
 Abstract Abstract
 PDF PDF
- Multiple endocrine neoplasia 2A (MEN 2A) is an autosomal dominant disease that consists of medullary thyroid carcinoma (MTC), pheochromocytoma and parathyroid hyperplasia. The activation of germ-line mutations in the RET proto-oncogene are responsible for MEN 2A. We describe here a rare case of MEN 2A in a patient who presented with an acute catecholamine-induced cardiomyopathy with cardiogenic shock and acute renal failure. The patient was diagnosed with pheochromocytoma and MTC associated with MEN 2A, which was confirmed by the detection of a RET proto-oncogene mutation at exon 11 on codon 634 (Cys634Arg). During familial screening, the patient's younger sister was found to have a benign thyroid nodule. Re-evaluation of this thyroid nodule revealed MTC with the same gene mutation. We also provide a review of the relevant literature.
- The Association between the Depression and the Perception of Obesity by Adolescent Girls.
-
Moo Jung Park, Eun Ah Lee, Sang Ho Lee, Jong In Kim, So Yeon Ryu, Ki Soon Kim
-
J Korean Endocr Soc. 1997;12(2):295-307. Published online January 1, 2001
-
-
-
 Abstract Abstract
 PDF PDF
- BACKGROUND
This study was performed to find the association between the depression and perception of obesity by adolescent girls in Jung Eup City, Chollapukdo. The data were collected by questionnaire from July to October, 1996. RESULTS: 1. While the obesity rate of the girls by BMI criteria was 6.0%, 41.1% of girls perceived that they were obese. 2. Forty-eight percent of respondents tried weight control already, and as the method of weight control 33.3% tried exercise, 27.2% reduced food, 23.6% avoided snack before going to bed. 3. while 39.3% among those whose BMI was lower than 20 and 54.2% among those with BMI 20-24 tried weight control, only 5.1% among those who perceived their bodies as slim tried weight control. 4. By the analysis of self-rating depression scale (SDS) only 14.8% was normal without depression and the rest showed high SDS scale; 36.9% as mild, 38.5% as moderate, and 9.7% as severe state of depression. 5. While no statistically significant difference of SDS scores by the size of BMI was shown, significant different of SDS scores was shown among groups with different perception of their obesity and practice of weight control. 6. As a result of stepwise multiple regression analysis, dieting, perceived body image, and body mass index were significantly associated with depression of the adolescent girls. CONCLUSION: Adolescent girls who perceived themselves overweight regardless of actual weight were more likely to diet than other girls. And these characteristics had an influence on the depression of the adolescents. It is suggested that appropriate education should be required to prevent thoughtless weight control of the adolescents and to maintain mental health of the adolescents.
|